Multidisciplinary Poster Session -
Nursing & Public Health
held on April 24, 2025 at the Lander University Academic Symposium
Faculty Sponsors: Liz McDowell - Claire Mensack
Presenters: Ann Ryan Alexander - Katie Darmer - Kyra Osten - Olivia Morgan Price - Aurie Riggins - Kaliyah Washington & Iyana Kelly
Scroll to view all projects!
-
![]()
Ann Ryan Alexander
Click here for a closer look at the poster.
The Effect of Diabetes Mellitus on Mental Health
The prevalence of diabetes mellitus continues to rise globally, with approximately 37 million Americans affected. Individuals with diabetes are 2 to 3 times more likely to experience depression, yet mental health concerns in this population often go undiagnosed and untreated. This project explores the correlation between diabetes management and mental health outcomes, therefore emphasizing the need for integrated psychological support in diabetes care. Research highlights the impact of socioeconomic status, diet, and external stressors such as the COVID-19 pandemic on mental well-being in diabetes patients. Evidence suggests that strategies like mindfulness-based stress reduction (MBSR) and professional counseling can reduce anxiety and depression and improve overall coping strategies. To improve outcomes, healthcare providers should implement mental health screenings during routine diabetes care and establish peer support groups for patients. Interventions like these enhance self-management skills and provide a sense of community for these individuals.
Ann Ryan Alexander is a senior nursing major with a minor in public health. She is a part of the Honors College and the Lander University Student Nurses Association. In Spring 2024, she completed an internship with the Self-Regional Diabetic Education Center. This project was inspired by observing patients there struggling with balancing diabetes care and mental health issues related to managing their diabetes.
-
![]()
Katie Darmer, RN, BSN
Click here for a closer look at the poster.
Improving Consistency of the Orientation Process in Labor and Delivery through Implementation of a Preceptor Class
Background: On-the-job training is an important aspect of the new graduate nurse experience. The new graduate registered nurse (NGRN) is paired up with a preceptor who is tasked with acclimating the new nurse to the floor. Training a new nurse is a huge task for a preceptor to undergo as it involves incredible foresight and skills to effectively manage this workload.
Problem: An extensive assessment survey of Labor and Delivery microsystem at Self Regional Healthcare in Greenwood, SC, revealed many inconsistencies among preceptors when orienting new graduate registered nurses (NGRNs). Staff were given minimal training to become a preceptor. When NGRNs are not consistently trained, critical thinking and clinical judgment skills suffer.
Methods: Following a literature review on how to best orient and educate newly employed nurses, a Preceptor 102 class was developed and presented to the nursing staff. Staff were introduced to Tanner’s Clinical Judgment Model (TCJM) to streamline the orientation process. They were reintroduced to Lasater’s Clinical Judgment Rubric (LCJR) and introduced to Keith RN’s Clinical Judgment Rubric (KRNCJR) to use in evaluating clinical judgement skills. A new tool, Darmer Orientation Tool (DOT), was developed to promote consistency among preceptors. With the tool, staff were able to monitor the progress of the NGRN’s clinical judgment skills. By introducing all staff to the new tool, the staff were united to improve the consistency of the orientation process.
Interventions: A “Preceptor 102” class was developed to improve consistency amongst preceptors in the labor and delivery. The class educated the staff on TCJM, LCJR, and KRNCJR. The staff were introduced to the DOT tool. The staff were given a survey before and after instruction to determine effectiveness and implications for future practice.
Results: Ten participants were initially enrolled in the study; eight participants completed the study. Results showed that staff saw value in the new orientation tool and planned to utilize it in practice when orienting NGRNs. Following the intervention, half of participants stated that critical thinking skills were important to teach. Preceptors were able to list skills and techniques to help NGRNs improve their clinical judgment and critical thinking skills. Most preceptors (87.5%) stated that the KRNCJR was helpful to learn and the DOT will help improve the consistency of the unit orientation process (75%).
Conclusions: As a result of this study, preceptors saw value in preceptor training and implementation of the DOT. Further studies should determine validity and reliability of the DOT and follow NGRNs through the entire orientation process to ensure consistency was achieved.
Katie Darmer, RN, BSN, RNC-OB, C-EFM, CLC, is a graduate student in the Clinical Nurse Leader program, Nurse Educator Concentration at Lander University. She has worked as a staff nurse at Self Regional for the last 13 years before making her transition to teaching at Lander University. While employed at Self Regional, she spent a majority of her time precepting new graduate nurses and was the recipient of two DAISY awards. She is currently employed full time at Lander University as a Clinical Instructor. Her work as a preceptor and her passion for teaching inspired this project and presentation.
-
![]()
Kyra Osten
Click here for a closer look at the poster.
The Effect of Frequently Repositioning Immobile Patients and the Development of Pressure Injuries
Pressure injuries (PIs) are a significant challenge in healthcare, particularly among immobile patients in intensive care units (ICUs), where incidence rates range from 6.6% to 36.8%. This study explores the effect of frequent repositioning on the development of pressure injuries over two months. Current clinical guidelines recommend repositioning patients every two hours in bed and every one hour in a chair, with additional offloading and weight-shifting strategies to relieve pressure on bony prominences. Despite these recommendations, inconsistencies in clinical practice persist due to limited evidence on the optimal repositioning frequency and variability in individual patient needs. The study highlights the critical role of nursing staff in PI prevention and underscores the need for improved knowledge, attitudes, and practices to mitigate PI development. Findings suggest that consistent, evidence-based repositioning protocols may enhance patient outcomes and reduce PI-associated complications such as cellulitis, osteomyelitis, and bacteremia. Future research should focus on establishing more definitive guidelines tailored to patient-specific factors to improve clinical outcomes and patient care standards.
Kyra Osten is from Spartanburg, Sc and a senior nursing student whose achievements include being the secretary of LUSNA, and interning at Spartanburg Regional as a student nurse intern (SNI).
-
![]()
Olivia Morgan Price
Click here for a closer look at the poster.
Pain Management for IUD Placements
Intrauterine devices (IUDs) are a common form of long-term birth control for women, with an estimated 159 million users worldwide. Despite the invasive nature of the insertion procedure for IUDs, pain management is not routinely offered to patients as a standard of care. It is the role of healthcare professionals to advocate for their patients and ensure the best care is provided. Research was conducted with this question in mind - For women seeking birth control, does optional anesthesia administration before IUD placement improve patient comfort and satisfaction as compared to limiting the use of pain management? Current studies on this topic were reviewed and analyzed to provide insight into IUDs and their effects on patients. Also included was a current agency policy from the Centers for Disease Control and Prevention (CDC). The results of this research concluded that the use of pain management was effective in helping patients overcome a crucial obstacle in seeking birth control. It was also found that providers, who often underestimate the pain experienced by their patients, should provide more detailed and transparent patient education on the procedures they perform. Further development and research into the practice of IUD placements are required to ensure patient comfort and satisfaction.
Olivia Morgan Price is a senior nursing student and a member of the Honors College from Gilbert, SC. On campus, she is a part of the Lander University Student Nurses’ Association and the Honors College Leadership Council. After graduating, she plans to work as a travel nurse before pursuing graduate education.
-
![]()
Aurie Riggins
Click here for a closer look at the poster.
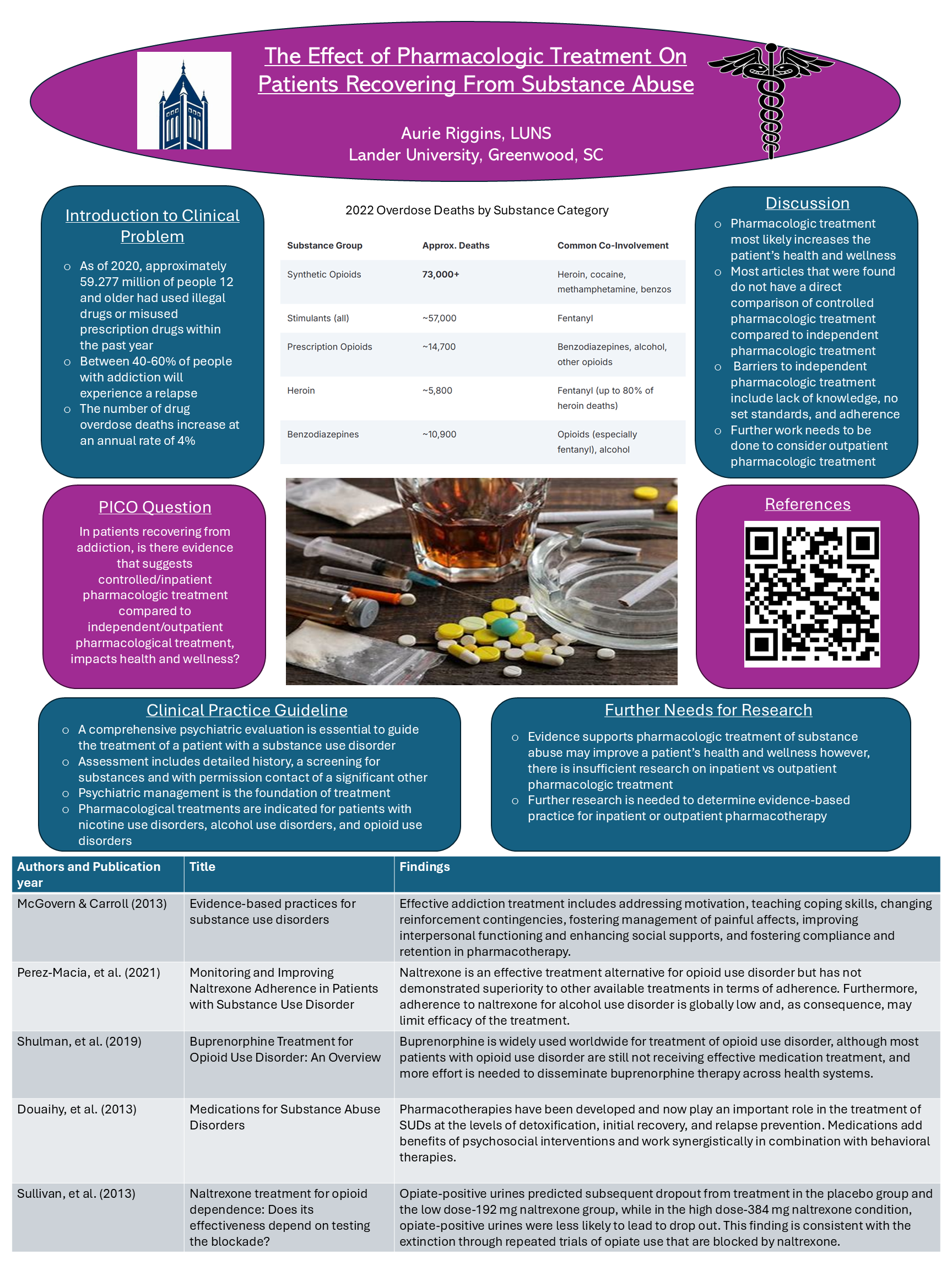
The Effect of Pharmacologic Treatment On Patients Recovering From Substance Abuse
A shocking 27.2 million Americans aged 12 or older reported battling a drug use disorder in the past year. In the year 2022, there were approximately 108,000 total overdose deaths in the U.S. and that number increases at an annual rate of 4%. Research shows that addiction is treatable, and recovery is possible with success rates of up to 50% with medication assisted treatment. This project investigates whether, in patients recovering from addiction, there is evidence that suggests controlled/inpatient pharmacologic treatment compared to independent/outpatient pharmacologic treatment impacts health and wellness. A literature review of current research on the topic was conducted of peer-reviewed articles written within the past 10 years. Five relevant articles were found in the CINAHL and PubMed databases using key words “substance use” and “pharmacologic treatment.” The results of this literature review were inconclusive. A gap was discovered in our knowledge concerning inpatient treatment compared to outpatient treatment of substance use disorders, and more research is needed in order to better inform healthcare best practices.
Aurie Riggins graduated from Pendleton High School in Pendleton, SC and is a senior nursing major. Her achievements include working as a peer tutor on campus, being a member of Lander's Honors College, externing at AnMed Health the summer of 2024, and being a member of Sigma Theta Tau nursing honor society. After she graduates in May, she plans to work as an emergency nurse.
-
![]()
Kaliyah Washington & Iyana Kelly
Click here for a closer look at the poster.
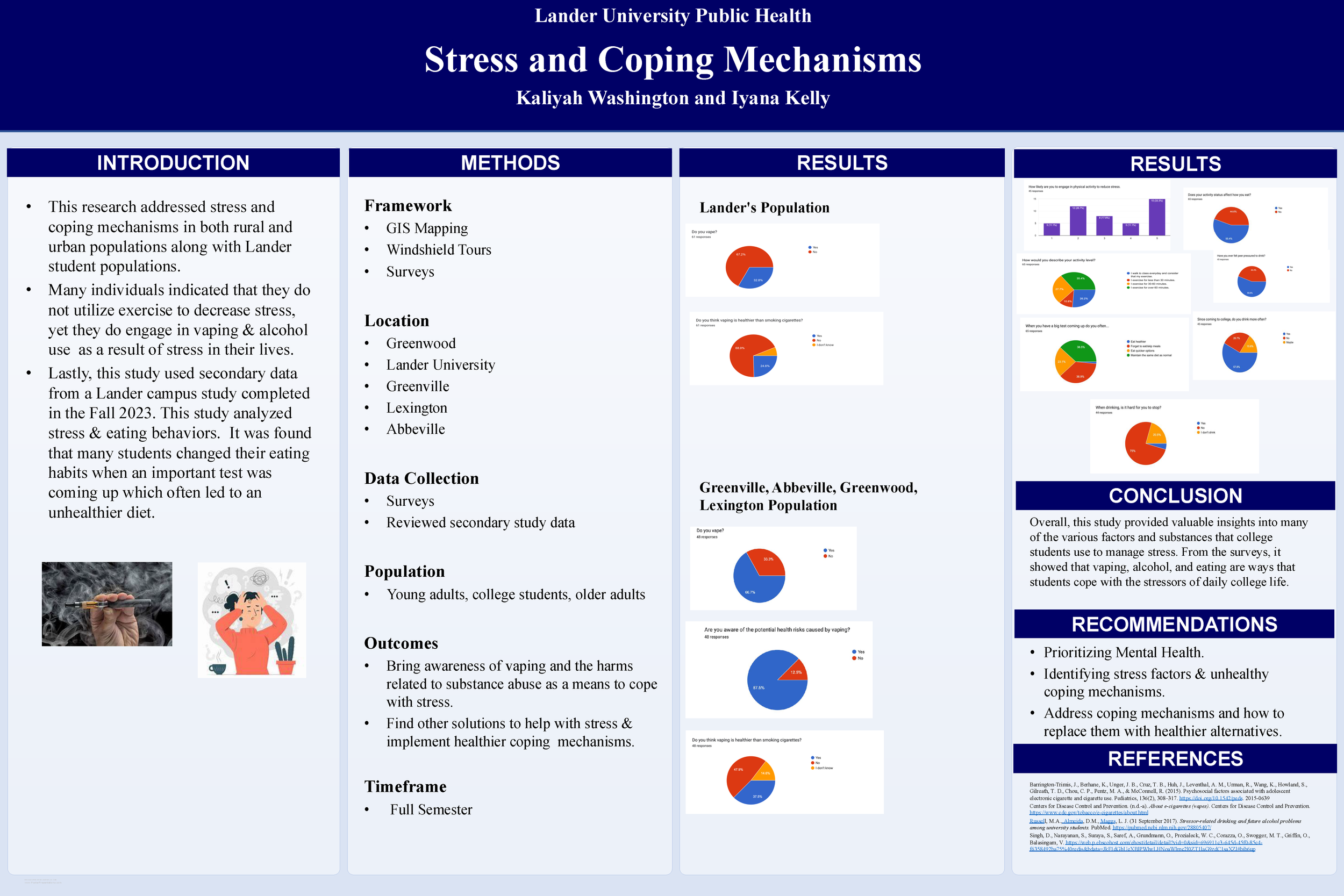
Stress and Coping Mechanism
This research poster addressed stress and coping mechanisms in both rural and urban populations along with Lander students' population. This study used GIS Mapping and Windshield Tours as a way to collect data along with multiple surveys that were conducted in various populations. This poster will also show how not many people utilize exercise as a way to decrease stress, but how vaping use has increased among communities. Along with vaping, how in the college years drinking has been an uprise for a coping mechanism. Lastly, this study used data from a previous study done in Fall 2023 that analyzed stress and its effect on eating. From this study, it was found that many students changed their eating habits when an important test was coming up which often led to a more unhealthy diet. From all these results, this class suggests that there be more programs focused on how to manage and deal with stress and addiction.
Iyana Kelly graduated from Camden High School in Camden, South Carolina and is a senior public health major at Lander University. Her achievements include being a supportive Resident Assistant on campus and also having the honor of being on the Dean's List.
Kaliyah Washington graduated Sumter High school in Sumter SC. She is a senior Public Health at Lander University. Her achievements range from networking with coordinating events and more. She's also been on the President's List last semester.